Wise Grandma Gloria


Grandma Gloria is taking care of her sick grandson without much fear of being infected with the flu virus. She knows that the flu virus is easily spread and that any contact with an infected person is risky. But what else does grandma know? His grandmother knows that the vaccine she has received protects her from the disease so she can fully devote herself to her grandson’s care.
What is a vaccine?
A vaccine is a preparation that contains dead or weakened bacterial or viral pathogens or only essential immunogenic parts thereof. The role of the vaccine is to create a memory in the cells of our defense system when encountering a pathogen similar to one that causes serious disease in nature. When the organism naturally gets in contact with the pathogen it was vaccinated against, our response of our defense system will be faster and stronger than if we did not receive the appropriate vaccine and thus protect us from the disease.

Vaccine - random discovery
Edward Jenner and Louis Pasteur developed the first vaccines before they even knew what the viruses were. At the time (19th century), the electron microscopes, under which viruses could be seen, weren’t even invented. Still, Jenner noticed that women who milked cows rarely got infected with smallpox He continued exploring and found out that they often got over cowpox - a milder disease caused by a related virus. The immunity they gained protected them from deadly smallpox. This discovery helped Jenner develop the first effective smallpox vaccine that saved millions of lives. This immunization process was called vaccination (Lat. vacca, cow; that is, vaccinus, from the cow) and the term was subsequently accepted for all immunization procedures

Source:
Blaisedell, Albert F. (1904.) Our bodies and How We Live,
Boston: Ginn &Company, page.189
How was the first vaccine developed?
In 1796, the British physician and naturalist, Edward Jenner, took tissue sample from the hand lesion of a dairymaid who had cowpox and vaccinated it into a healthy eight-year-old boy. The boy developed symptoms of fever and loss of appetite, but he recovered quickly. Therefore, Jenner decided to perform an even riskier experiment. He repeated the vaccination, but this time with a substance of freshly damaged smallpox-infected skin tissue. The boy did not develop the disease, and Jenner discovered a vaccine which brought an end to the smallpox epidemic.
Find out more about the first vaccine in video.
Source - author: youtube.com - OpenMind


Are viral vaccines different?
Although we might not think so, there are many different types of viral vaccines. Vaccines differ in whether they contain live attenuated viruses, fully inactivated viruses or only parts of viral particles (subunit vaccines). They also differ in whether they are produced by traditional or modern technological processes such as genetic engineering.
Each type has its advantages and disadvantages. Vaccines with live attenuated viruses contain weakened viruses that do not cause the disease but stimulate the response of the defense system most similar to the response to the natural infection with the virus. Therefore, such vaccines provide quality and usually long-term protection against disease.
Vaccines with inactivated viruses contain viruses that cannot be replicated because they have been inactivated by some suitable physical (e.g. high temperature) or chemical process (e.g. formalin). Such preparations stimulate a weaker response of the defense system than the response to the natural virus infection, so the vaccination should be repeated two or more times.
Vaccines that contain only parts of the viral particles may vary depending on the method of production. Their common characteristic is that they do not contain whole viral particles, but only proteins present on their surface. Such preparations also generate a weaker response of the defense system than the response caused by the natural viral infection, so the vaccination should be repeated.
Find out more about the types of vaccines and how they are made at:
Find out more about diseases from which vaccines protect us at:
And what type is the flu vaccine?
Subunit vaccines or those containing inactivated viral particles are generally used to help protect us from the flu. There are also vaccines with live, attenuated influenza viruses.

Spray vaccine
On the world market, a nasal spray vaccine can be found. The virus in this vaccine is alive but altered so that it cannot infect the lungs and cause severe symptoms of the disease. How? Scientists have figured it out - they have exposed the virus, for a longer period, to temperatures lower than the body temperature in our lungs. Fighting for its survival, the virus began to accumulate mutations which allowed it to adapt to life at a lower temperature. Thereby, the virus has lost its ability to replicate in the lungs, but it successfully replicates in the cooler environment of the upper respiratory system, where it does not cause disease but successfully activates our defense response.

What does vaccine contain,
i.e. Grandma’s weapon against the flu?
The most significant part of the viral preparation contained in the flu vaccine are the viral glycoproteins that our defense system recognizes as "enemies". After the first contact with them, our defense system will "remember" what the "enemy" glycoproteins look like so that the next time our system will be ready to defend our body. Each time a virus with the same combination of glycoproteins is found in our body, our immune system will recognize it and prevent the development of the disease. In that way, Grandma's body was prepared for the virus!
What happens in our body when we get vaccinated?
On the surface of the virus, natural or contained in the vaccine, there are molecules, called antigens which stimulate a response of our defense system. When encountering viral antigens from a vaccine, the body develops an immune memory that encourages a faster and more intense defense response when re-encountering the same antigens.
Find out more about how the vaccine works at:
Why Grandma gets vaccinated every year?
The flu virus is specific for its expressed variability, that is, the emergence of new variants and the combination of different glycoproteins. Because of this, scientists are changing and adjusting the composition of the vaccine every year to make it more effective. What does that mean? Only the vaccine containing the glycoproteins of those viral variants that could infect us in certain seasons will be effective because the viral glycoproteins with which our body has not been in contact will not be recognized. Before the production of the vaccine, it is necessary to identify the viral variants that currently prevail in the world each year and to predict the possible viral combinations for the next season. To create protection on time and to be ready for the new flu season, we need to get vaccinated every year! At least for some time...
The number of people affected by the flu is increasing every year. To finally end seasonal epidemics, scientists are working on a unique solution in the form of a "perfect" vaccine.
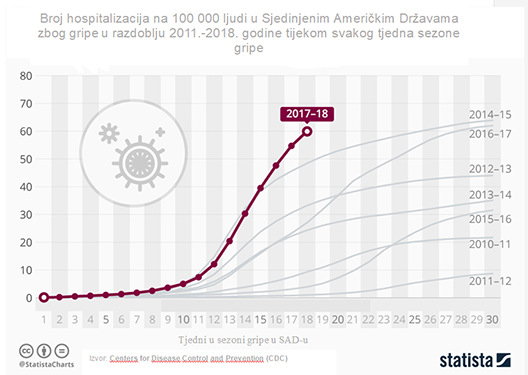
The description (graphic representation) is below the picture: The number of people suffering from influenza in the US has been increasing since 2011, when the number of hospitalizations was 10 per 100,000 people, while in 2018, that number was nearly six times higher. This indicates that there is a need for a universal flu vaccine development.

On the trail of the perfect vaccine

Scientists are working diligently to create a universal flu vaccine that would protect us from viruses with different combinations of glycoproteins for a long period. How is that possible? Certain viral proteins are common to different viral variants. Their detection and isolation, then the preparation of an effective vaccine that contains them would provide protection against infection caused by many variants of the influenza virus. Even though it sounds simple, this task is not easy at all! Inspired by this idea, scientists at the University of Oxford are on the trail of the vaccine of future discovery. Recent studies have shown that some parts of hemagglutinin and internal proteins occur in different variants of influenza viruses. Stimulation of the immune response caused by these common antigens is one way of generating immunity to multiple variants of the causative agent.
Learn more about the “perfect” vaccine.


An egg a day keeps the doctor away
When needed, one egg contains millions of viruses!
Did you know that the easiest and cheapest way to replicate the influenza virus needed for mass production of vaccines is in fertilized chicken eggs? This vaccine production technique was first applied by E. W. Goodpasture, an American physician, back in 1931 and it still plays an important role in the creation of vaccines against certain viral diseases.
Did you know that the whole process - from the choice of viral variants that the vaccine will contain, to the delivery of the vaccine - can take up to eight months?
More about the flu vaccine production process.
Source - author: youtube.com - Wellcome Trust